Here we are… past the terrible two’s (and three’s), a whole pandemic and purchase and renovation of a home (while pregnant), and a now two year old. The last time I wrote on here, George was 2 days away from his lip and tongue release procedure. I remember that morning so vividly, as Richard and I were driving into the city the car was pretty quick and anxiety levels were high (on my end at least!). Richard has always carried stress with so much more grace. It felt like we were in there for ages, but with George’s weight, the first dose of sedative did not take, so we had to give it another go. It took 5 people to hold George down during the procedure and I was in tears the entire 3 minutes. First, the doctor released his lip tie and then laser cut his tongue tie. George case was so severe that he requires stitches in order to prevent reattachment. Being that George was a frequent visitor in hospitals and doctors, I did not think I would have a hard time, but no one ever prepares you for these things. Post procedure the doctor came in and explained that George was in fact the most severe case he has seen in his career, which blows my mind until this day that no one caught it. We did all of the exercises they taught us for two weeks and resumed business as usual.

A month after George’s procedure, we found out we were pregnant with a little boy and life slowed down dramatically as the first trimester took over my body. All I wanted to do was sleep and eat blueberries, but George continued to push through his therapies until his 3rd birthday. Once George turned three, he phased out of early intervention and our town school district took over his education. They initiated his IEP (Individualized Educational Plan) and set up goals after they did all of their evaluations. At this point, COVID was still very much around and I did not feel comfortable sending him in due to his heart condition. This meant that George needed to attend school virtually… this is hard enough with any child, but with a child that has issues with attending and focus, it is nearly an impossible task. We had support at home, as Richard and I were both working full time from home.
2021 rolled around and boy did George know how to ring in the New Year, we were all at home hanging out and Rich was lying down on the bed. George decided to jump on Rich’s back and lost his balance. George fell off the bed and I heard him cry like never before. He has always had a pretty weak and soft cry, but we did not know whether it was the shock of him falling or whether he was in pain. We put him in bed and gave him Tylenol. George is a pretty active kid, so the only way we could get him to lay in bed to rest was by letting him watch some TV. After two hours, I went in to get him ready for bed and he really struggled. I could tell it hurt him to move his arm above a certain point, so getting dressed was not even an option. It was January and COVID was very much still around and we were not vaccinated at this point, so Richard decided there was no way I was stepping foot into the hospital if I didn’t need to. My mom went with them and after an X-ray, the doctor told us that George had a broken clavicle and that it would take 4-6 weeks for him to heal. He was sent home with a sling, which of course did not look at all comfortable for him. The next day I went out to the pharmacy and did some modifications to his new sling. I let him sleep with us for a few days until we felt he was okay to sleep on his own. We had to limit his activity, which was a task in itself because as I said, George is very active. After 4 weeks, we visited the orthopedic, and he confirmed that George was fully healed!

One of the most dreadful times of the year had caught up to us. George had his annual cardiology appointment in March. These appointments are long and exhausting. I do not think it will ever get easier walking into the hospital to check the progression of his heart condition. Richard still finds it difficult and there is mental preparation that has to go into these appointments every year. Nothing had really changed since the last time he had his echo, but the doctor did mention a medication called Losartan. She said that doctors have been using this medication to slow down the growth of the aorta and that although there is no guarantee, the risks are very low. It made us so uneasy to even consider putting our 3 year old on heart medication, especially since he is not showing any signs of being at risk at the time. George has no restrictions, so we decided to put a pin on it until at least the next time he had to be seen.
After we found out we were pregnant, I constantly felt in a panic. I felt like we did not have enough space so that we could all maintain our sanity, so after many discussion and me pushing we decided to start house hunting. Of course, it was the worst possible time to buy a home, and it was definitely no time to be picky. And boy, are we picky! After 4 bidding wars, we finally had an offer accepted in March. We were well aware that our home needed an extensive amount of renovations.

These days we were staying so busy trying to figure out how we were going to furnish a whole house. Moving from a one bedroom apartment to a 4 bedroom house was no cake walk. We were spending most of our weekends going to different stores and looking for little bits. One Sunday night in late March, I felt something wasn’t right. I told Richard before I went to bed that I was not tracking the baby’s movements and I felt that he was not moving much. I thought so carefully about how to articulate because any type of scare makes Richard extremely uneasy. I reassured him that everything would be okay, and we went to bed. Babies tend to be more active when you’re trying to sleep, so I figured he would wake me up at some point, but by 3AM I had not felt anything. It broke me having to wake Richard up to tell him I felt we needed to call the doctor. I called the OBGYN office to let them know what was going on and the doctor called me back instructing us to go to the emergency room. We woke my dad up to ask him to keep an eye on George while we went to the hospital. By this point, Richard and I were both vaccinated, but they took the COVID test and thankfully, the doctor was waiting for us. We heard the heartbeat, but he was struggling to get the baby to move. Richard’s heart sank as the doctor made casual conversation with us for 15 minutes. Until this day, he tells me those seemed like the longest 15 minutes for him. He finally blurted out, “is the baby okay?” The doctor reassured him that he heard the heartbeat within the first few seconds of the ultrasound and he had no concern whatsoever. He also told us that sometimes, like us, babies have lazy days where they just want to rest. So we were sent on our way.
That same month my dad mentioned one weekend that he was having a lot of chest pain. If you have ever had the chance to meet my dad, you know he never complains, so I took this very seriously. The next day I dragged him to the ER where we spent hours. They did all an EEG, an echo, and a bunch of other exams. Because it was a weekend, the cardiologists were not as readily available. They ended up telling us that my dad would need to stay overnight to be monitored. I didn’t want to leave that hospital without knowing what the next steps were. My mom works at the hospital he was at, but she was away on vacation. The last thing we wanted was to scare her or have her cut her trip short and once we found out my dad would be placed on the floor she worked on, we decided to change the emergency contact on file. Since they have different last names, none of my mom’s co-workers knew who they had as a patient. I called the hospital very early the following morning to see if there was an update and to ensure my dad was being attended to. I picked him up and we called my mom to tell her what we were told. My dad would have to return to the cardiologist’s office the following day so they could conduct a stress test. Essentially, my dad would get leads put all over his chest and they’d put him on a treadmill for a few minutes at different inclines and speeds. He failed the stress test within the first few minutes, so it became apparent that there was an issue. My dad was scheduled for a cardiac catheterization. I can’t even begin to describe the feelings that came over me as my mom and I were in the waiting room during that procedure. The doctor came out, looked at us and said, “your daughter saved your life. We had a place a stent in your left main artery because there was 95% calcification. You could have gone into cardiac arrest at any moment.” My jaw was on the ground thinking to myself how he endured this chest pain for so long. His first question, while obviously still so loopy from the meds, was, “Is it my fault my grandson has a heart condition?” Oh my goodness. I could not have been more broken because he probably doesn’t even remember asking that question, but I’ll never forget it. From then on, my dad has lost weight and made an effort to be more conscious about his health and gets checked on annually by his cardiologist, which has now become the family cardiologist.
May rolled around, and I was 7.5 months pregnant when we closed on our house. I was in full nesting mode and although we knew what we were getting ourselves into, WE DIDN’T! Richard and I were trying to get everything sorted before our July 4th due date. We were running around trying to find a general contractor, plumber, electrician, architect and trying to design every little crevice of our house. Richard and my dad started demolition on the house and by end of June, construction finally began. We basically lived at Home Depot and Lowes for that month.

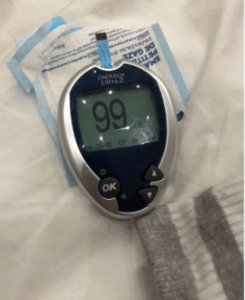
I guess in a way, it was great to have a distraction while I was pregnant, because although it was all overwhelming, it took my mind off of the stressors. Because I was high-risk with George and ultimately had preeclampsia, the doctor suggested that I take aspirin and monitor my blood pressure regularly during this pregnancy. My blood pressure during this pregnancy was often really low and I cannot tell you how many times I called the doctor’s office to ask them whether it was normal. I woke up feeling dizziness nearly every morning and it was difficult to get going. They consistently told me that it was okay and no cause for concern, but given my previous experience. By 36 weeks, the doctor instructed me that she wanted me to stop taking aspirin and my C-section was scheduled for June 28th. We were four weeks away from having a baby and tensions were running high. Richard and I were running around getting materials for our contractor, driving George to therapy 3 times a week, going to weekly appointments to check in on baby, and trying to keep up with our full time jobs. Richard has always been such a huge support for me. If you know me personally, you know that I am very much Type A and I love planning. If you have ever been pregnant or had a pregnant partner, you know that baby brain is a very real thing. I was forgetting and struggling to stay on top of things, and without me asking, he took on so much of what our family needed during this time.
We were getting ready to meet our little boy and finalizing a plan for George for the 4 days that we would be in the hospital. The last week was so hard for me emotionally. I would find myself crying so much thinking that this is the last bit of time that I would get with George as an only child. This broke me time after time. Richard and I always felt that we needed to wait to have children not only to heal, but also to give George our time and attention. It was hard to think about having another child when George needed us so much. I stayed in bed hugging George a little bit longer and squeezed him a little bit harder that week. Sleep was so hard at this point and the night before my C-section, I could not sleep. The morning of, I kissed George on his forehead as he slept while wiping the tears off my face trying my best to not wake him up and we head off to the hospital.

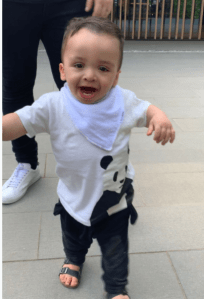
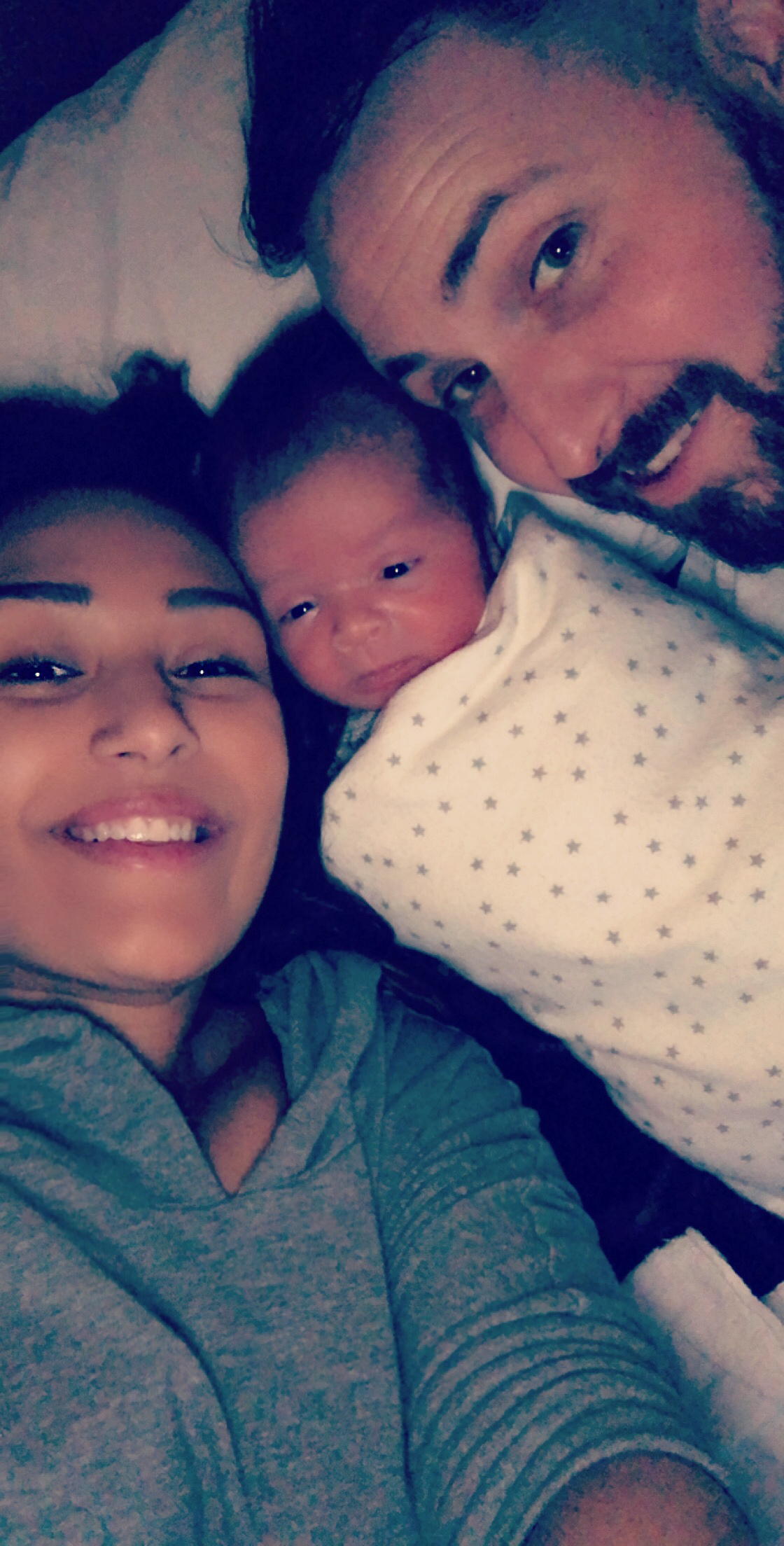
Jack had finally arrived and our experience was so magical. Our doctor made sure to make his birth so beautiful and positive which was so far from what we had gone through with George. George had the time of his life and my mom was sending me updates during our entire stay. He went to the zoo, to the Crayola factory, to the beach and Richard left for a few hours while my mom stayed with me to take him to the toy store. Those 4 days of Jack in the hospital were so special and what our hearts truly needed. During those four days, George’s speech exploded! I was so shocked when we came home; he was saying things unprompted and communicating like never before. I mean, I will be honest; he was not necessarily thrilled and was a bit confused as to why Jack was extending his stay.

Richard’s parents were due to come for the birth, but because travel was still very much affected by COVID, they were denied travel in the UK despite of all the documentation we had stating I needed the support post-op. It was so heartbreaking as it had been so long since we had seen each other (Jan 2020). That summer was quiet, but fun. I was on maternity leave and I truly enjoyed my time with the boys, by the pool, going on walks, going to the zoo and carnivals, all while trying to finish renovations in our home. George could not start school in the new town due to our house technically being inhabitable, so we started school in September we were currently living. I’ll never forget the day our home passed all inspections, November 8th, the same day the US opened the borders for travelers that had COVID vaccinations, Rich’s parents were on their way. Their visa had been cancelled due to the incident in June, so they had to wait a day to have it reissued, so on the following day, they got to meet Jack and finally see our new home. I started working on the school transfer paperwork and I cannot tell you how nervous we were to move him. We had gone through so many transitions and George had struggled with sleep for the first 3-4 months of Jack being born. The last thing I wanted was another change for him, so we decided to wait until after thanksgiving to move him over. On top of that, during the process of completing the paperwork I found out that the school he would be in would cater to children ages 3-21. I would stay up at night wondering how I felt about this and how scary it is to think that my 4 year old would be in a school with kids that are so much older than him.
In August, we went back to the developmental pediatrician. If you remember back from last year’s post, he was the one who reassured us that he sees no signs of autism and told us to keep an eye out for ADHD as George does seem to get bored with certain things and gets distracted easily. A year had gone by since and George’s focus had not improved at all; however, the outcome was not any different. The doctor told us George is too young for any type of medication intervention for ADHD and he had an expressive language delay. Like the first time, I was not sold. If there is one thing I have learned about our journey with George is that I will never take “no” or “not possible” as an answer. Of course, I can find myself going down a complete rabbit hole. I start to consume myself trying to find more information or answers. Richard knows how to ground me when I get like this and he asked that we give George more time as we have moved and he is going through several transitions. That is exactly what we did.
Richard and I had the chance to tour the new school before George would start and as soon as we met the teacher we absolutely loved it. The principal was so reassuring and everyone was so friendly. The teacher explained that her class consisted of children that required services and neurotypical children that would model behaviors for the other children. We felt this was so amazing for George because he would be exposed to playing with peers and practicing social skills that were hard to work on during COVID, so George started in his new school in December 2021.

That same month, Richard’s paperwork was finalized for submit for his green card. We had been working with the lawyers since July to get the package together because if you have ever gone through the process, you know it is a process. We had been married for 4 years already and we were dreading going through this, but it was time. Going through the green card process, we knew that we would not be able to travel outside of the US, which if you do not know Richard’s family all lives in the UK. We did not want to be restricted from travel; however, we were told that as long as he had his advanced parole (which typically takes 5-7 months), we would be able to leave the US. We were trying to stay positive about the processing time.
2022 was here and even thinking about it now makes me cringe. My maternity leave was coming to an end and it was getting harder and harder for me to accept. I told Richard that I would not send Jack to daycare as long as I am breastfeeding, and I did not intend to stop any time soon at this point. I was going back to work beginning of January and I had no idea what I was going to do, so my mom offered to go part time at her job to help me at home. My sleep was so disrupted every single night because even though Jack was 6 months at this point, he would never sleep through the night. He would wake up every night between 3 – 4 am to breastfeed. My brain fog made it difficult to stay on top of everything.
Soon enough, it was March. I was completely dreading this moment. Before COVID, we had seen a urologist who told us that George would need surgery, but of course, it was put off. So now it was time. I never imagine my child having to be put under anesthesia before myself, but there we were. I was so lucky to have my mother in law helping me through George’s recovery. Within two weeks, he was back at school.

A month later, I saw my OBGYN due to excessive bleeding that started becoming concerning. I kept telling myself it was hormones going haywire due to breastfeeding. But an ultrasound confirmed that I had polyps, so I was scheduled for surgery. Richard went with me and we were told by the OBGYN that the procedure to remove polyps was routine. Everything went well, until I got home. I went home and slept for a few hours, and when I got up, I noticed a significant amount of bleeding. I assumed this was normal, but after an hour, I told Richard. We ended up calling the doctor and she said to give it another hour or two. I really was not in the mood to go back into the hospital, but Richard pushed me to go. I called the doctor again and she told us the amount of bleeding I was describing was not normal. She told me to meet her in the emergency department, so my mom picked me up and took me. An hour later, I was having my blood drawn, my cervix numbed and stitched. The doctor explained that the tool used during the procedure punctured my cervix and was causing me to bleed out. She said the amount of blood would have been extremely dangerous and likely would not have made it to the next morning.
We had movement on the green card process. The first document was approved. Richard was approved to work in the United States. We still needed the advanced parole document to come through to allow us to travel.
I felt enough time had gone by and I just could not let go of the thought of what the developmental pediatrician said. I drove myself crazy looking for different doctors from neuromuscular specialists, neurologist, developmental pediatricians, neurodevelopmental pediatricians and alternative medicine. The waitlists for these kind of doctors are months, if not years long. We are still waiting for some of our appointments.
George had been in school for 6 months and before the end of the year, during a progress report meeting the teacher expressed she felt that the class was too overwhelming for George. She said she has seen progress, but that she feels he needs extra support, so although his IEP does not have a 1:1 aide, she has informally put one in for him. She further explained that she felt George had been doing so much better with the extra help.
A few weeks later, we had an appointment with a neurologist and she spent over an hour and half with us. I thought I would take the out of sight, out of mind approach this time and tried my best to start neutral. As we sat there, and she observed George, the words finally came out of her mouth. Autism and ADHD. She was so kind to point out all of George’s amazing qualities and strengths. As usual, Richard had several questions and the doctor reassured us that we have been giving George all the resources to help him be successful. I was quiet most of the appointment because I knew it my gut this was coming. The neurologist said that George would need to have an EEG and MRI done to ensure that everything is okay. We walked out of there and nothing felt different. Richard was the same. George was his happy self. As we walked to the car, I just broke down.
And that would be me for the next few weeks. I would hide away from the world, crying in whatever bathroom I could find. Richard was my rock during this time and he knew when he looked into my eyes the pain I felt. It took me so much of me to process and understand my feelings. I was not sad because my son had received a diagnosis of ASD and ADHD. I was sad because of how certain things will be hard for him. I was sad because people will see him differently. I started to think, “Will he ever get to the point where he’s conversational?”, “Will he go to college?”, “Will he find love or a life partner that will love and accept him for who he is?” As I put this down in to words, I feel as if I am reliving the feelings and it is still just as painful today. And it will be forever because ASD is unpredictable. It is good days and bad days. It is trying to play detective to figure out your child’s needs and patterns.

Between all my feelings, I had to remind myself I still had Jack to take care of. He was turning one a week after we received the diagnosis and I was still breastfeeding him. He was walking and it was getting harder on me, even with the help of my mom. George had already qualified for extended school year, which meant he goes to school for all of July and he would be off for all of August. We shared the information with George’s school and they said that since he has the ASD diagnosis, he would qualify to go into a different program. His IEP would be updated to state the new program and he would receive more services. Everything started moving quickly, and we were given the opportunity to meet the teacher of his new class. We were so nervous to move George into a new class, but we felt we needed to give it a chance. We knew he was struggling in a class of 16 children, so a class with 6 children would mean him receiving more support. By going into this ABA class, George would automatically receive 4 sessions of speech a week, in addition to 2 sessions of physical therapy and 2 sessions of occupational therapy. So it was settled, we decided this program would be best for George.

The summer was hard as I felt I was struggling to stay on top of everything. Working full time, taking care of Jack, consuming myself in wondering whether I am doing everything possible for George. I signed him up for private occupational therapy sessions, speech and aquatic therapy. I researched summer camps and tried to find a good fit for him, so we decided to do half day summer camp for four weeks in August. Two weeks of a social skills speech group, and two weeks of a sensory trampoline summer camp. Thankfully, by this time we had met our neighbor’s daughters. They helped us so much during the summer. They were incredible supportive and sweet with both boys. And when they come back from college, they always come over to help and spend time with us. The last week of August my mother in law came back to help with the boys before school started.
September had come so quickly. It was hard to think about how much we had done during the summer – beach trips, a trip to Washington DC, another to Virginia Tech. Jack was headed to daycare full time and we survived 14 months of breastfeeding. It was so heartbreaking, but freeing.

We had already received news that George’s initial EEG came back abnormal, which meant he needed to have a 48 hour in home EEG exam done. I had coordinated with the neurologist and cardiologist to have George’s heart and brain MRI at the same time. This meant that George would need to be under general anesthesia. Twice in one year, so before going back to school, he had the MRI done. I was so scared of how he would wake up. I could not stop thinking about the first time he woke up from general anesthesia; he was so disoriented and upset. This time it was a completely different experience. His cardiologist said that George’s heart function was great and she reminded us that she thinks he would be a perfect candidate for medication to prevent the growth of his aorta. We did not hesitate this time and decided to start the medication. In regards to his brain MRI, the neurologist told us that George’s frontal lobes were misshapen and that his brain was pressing against his optic nerves. I had so many questions. What does this mean? Why are the frontal lobes misshapen? Could this explain the ASD or ADHD? She told us that she had never seen anything like that in her entire career and that she does not necessarily see a correlation; however the frontal lobes are responsible for expressive language, executive function, and self-control. She told us that it would likely have something to do with the ADHD, but not the ASD. In addition, she told us that we may want to have George’s eyes checked to ensure he doesn’t have any optic nerve related conditions. I was not sold. I did not like the fact that things felt vague, so within that same week I made an appointment with another neurologist.
The neurologist was shocked that I was sitting in his office and we had to go through George’s medical history and various questions. Two hours later, he said he agreed with the diagnoses of ASD and ADHD. A week later, he called me to tell me he reviewed the pictures of George’s brain MRI with his entire team. “George has a congenital anomaly (something he was born with) involving the structure of the brain. This will not change over time. There was NO evidence of increased pressure in the brain so the large head circumference is related to the same cause as the autism or to another factor. He does not require any treatment of the large head or the MRI findings. There is no need to repeat the MRI unless his clinical condition changes, which we do not expect.” I am sure you can imagine how frustrating it can be not having answers, but I needed to get a second opinion. I had already taken George to see an ophthalmologist where he had to have his eyes dilated for them to do a thorough check. The doctor reassured me that George had astigmatism in one of his eyes, but other than that the doctor did not see any concerns with George’s optic nerves.
By this point, things were really starting to weigh on me, emotionally. I felt this immense amount of pressure to always keep myself composed and together and it was becoming harder and harder to communicate with Richard.
We did the 48 hour in home EEG in October. We took George in on a Friday afternoon to get all the equipment put on. He would had over 25 leads on his head and he would have to wear a backpack for 48 hours, even while sleeping. In addition, we would have to set up cameras in the two rooms where he spends most of his time, so that they can see whether George has any physical tics when and if he has absent seizures. I cannot tell you how nerve racking it was having him at home and watching his every move, and making sure that Jack did not pull any of the leads. I stepped out for a few minutes and I get a call from Richard to say that George pulled a few off. Oh my goodness! He told my mom to take the bandage off his head and quickly called the company, they were trying so hard to get the leads back into place. If enough leads came off, this means the test would need to end because they would not have a good read. The company confirmed that everything looked good. We were counting down the minutes to take all the equipment off and go out for some fresh air. George completed the 48 hours! A few days later, we get the call from the neurologist with the results. She tells us that George has extremely rapid brain activity and very often he has 1-2 second misfires, which means that he could be at high risk for seizures. Our first question was, “Is there anything that you can see from the video that correlates with when the misfires are happening?” We wondered whether it was him getting excited, watching TV, sleeping could provoke these misfires. She had us schedule an appointment with her to discuss next steps.

We were back in the neurologist’s office and the visits never get easier. Richard knows that I can handle going to most appointments on my own, but neurology is not one of them. The neurologist sat us down, showed us George’s EEG, and explained that there was not a specific trigger for the misfires. She tried to connect the video with the EEG and she was not able to find a correlation, but what she said is that his rapid brain activity is concerning. She told us that even while George is sleeping, his brain activity is very erratic. She went on to explain that because of his brain activity and quick misfires, she recommends two medications. The only thing going through my head was that my baby was not even 5 years old and he would have to be on heart medication for the rest of his life and now another medication? There were two options of medication. Both helped with stabilizing the brain waves and preventing seizures. One medication caused extreme moods and with many patients, anger. If you have ever met George, he is not an angry or aggressive boy. The other medication caused a severe allergic reaction, so it would be a long process to get George to the full dose. While sitting in her office, I had a flash back. In August, we went to Chipotle to grab a bite to eat. Richard was outside with Jack as George and I waited for our food to be ready. George was sitting at one of the tables when all of a sudden, he starts shaking uncontrollably. I took my phone from him and tried to get his attention and he would not stop shaking. I ran outside in a panic to tell Richard and I was beside myself. By the time Richard had come inside, it had stopped. I mentioned this to the doctor and right on the spot, we decided to go with the second option. We started the tapering process. It would take 6-8 weeks to get him to the full dose and by mid-December. Thankfully, George did not have an allergic reaction to the medication. He was taking four pills in the morning (heart and epilepsy medication) and 3 pills (epilepsy medication) at night. During the same appointment, she recommended that we do a whole exome genetic panel. She mentioned that it may give us some clarity as to why we are seeing this with George.

In late November, we received notice that Richard’s advanced parole was approved. 11 months of waiting. It was beyond bittersweet. This was everything we were hoping for. We had so many plans to fly to the UK immediately and going for Christmas, but we were not in the mindset to do so. We did not share the news with anyone for weeks as our focus was elsewhere.
If you have read George’s journey, you may remember us being offered this genetic testing many times, yet there is one piece of advice that we always fell back on. When George was born, he was immediately admitted into the NICU and one doctor said to Richard that going through with a whole exome genetic panel is like opening up Pandora’s box. So, our agreement was to always base our decision on whatever it was George was showing. When we were offered the congenital heart disease and pulmonary hypertension panel, we agreed to it because George has a dilated aorta and had pulmonary hypertension while in the NICU. When we agreed to the fetal overgrowth panel, we agreed to it because George was a large baby with a large head. Ever since, we felt that kept us on the right path; however, this time we knew it was our last genetic testing. No matter how scary it was. This was it. From there, we received our kits and George, Richard and myself all took swabs to send into the lab. You may be wondering why the parents have to send in samples. Well, if they find that George tests positive for anything, they want to check the parent sample to confirm it was not inherited from one of us. We knew the results would take around 3-4 months, so we tried to put it out of our minds until March/April.


The end of December was particularly difficult for me. I started to reflect on the year and it was so painful to think about. The guilt and weakness that came over me was debilitating. Richard was really there for me. I locked myself in our room for a few days and slept. And cried. The best way I could describe these feelings to Richard was that I just felt that I was constantly waiting for the next thing to happen. It was a relentless punch to the gut and I was just stuck in this negative headspace.
I did not have high expectations for 2023 because of how awful 2022 was. I say it was awful because it was such an emotionally draining year. It was hard for me to be optimistic, but felt that I needed to do it. There were so many beautiful things that happened in 2022, and the one thing I told myself was that I did not want to regret letting those moments pass me by. My family is overall healthy and happy. I told myself that my goal for 2023 was to not consume myself with my worrisome thoughts. This year I would not allow myself to go down the rabbit hole again and again.
In January, I had to travel to Kentucky for work twice and Richard had to travel to the UK for work. So Richard traveled with me to Kentucky both times and my parents watched the boys. We overate, went axe throwing, and went to whiskey distilleries. It was everything we needed. We decided to take the boys to the UK, which they absolutely loved. They spent one on one time with their grandparents and cousins, while being completely spoiled. Richard and I were able to go into the office to work. Jack was able to meet his great grandmother, which was the highlight of my trip. Jack is named after his great grandfather and it was the first time he was meeting our UK family.

In February, we had our annual cardiology appointment. George did great, and we received wonderful news. Since George had a heart MRI last September, the measurements are much more accurate and the cardiologist told us that his dilation is now considered to be in the mild range, as opposed to the moderate range. This was not to say that the medication he is taking is the reason for it, but nonetheless we will take the win! Later that month, Richard had to travel to Miami for a conference and my mother in law came to stay with the kids, so I could go with Richard. We both needed it after George being on spring break.

Not even two weeks later, we received a call from the neurologist. My heart sank when I saw her name come up on my phone. She said, “Hi, this is Dr. Cope. Is now a good time? We received George’s genetic results.” It was the call I was not ready for and dreading for months. I had called the lab before we went to Miami and they told me the results would come back mid-April, so I had pushed the thought out of my head. I ran upstairs with the phone on mute and tears running down my face to tell Richard it was Dr. Cope on the phone. He said, “It’s going to be okay, babe” and gently patted the bed to come sit next to him. He held me as the doctor started to talk, I took a deep breath. She began explaining that George’s report states that he tested positive for a PIK3CA gene, and it is likely related to a condition called MCAP (Megalencephaly-capillary malformation Syndrome). Obviously, like any parent, I start to google all of these words as she’s speaking and I see keywords, “tumor”, “growth”, and the C word. My world starts to slowly crumble. We ask a million and one questions about what it means for George. She proceeds to tell us that she does not know much about this gene; however from what she has read, it would explain George’s large head and brain, his developmental delays, and cardiac issues. She refers us to a genetic counselor and a follow up appointment with her. We hang up the phone and Richard is cool, calm and collected. I think my heart wanted to tell me to be sad, but my head was telling me that everything was okay. We were expecting so much worse and it seemed like we had answers as to what was going on with George.

Naturally, the next day I was on the phone with the Children’s Hospital at Columbia and Seattle’s Children’s Hospital. The world renowned doctor for PIK3CA was at Seattle’s Children’s, so that was my first attempt, but of course, Columbia is right across the bridge. When I called, it must have been my lucky day because they said they are scheduling out in July; however, someone must have cancelled because they have one appointment in April. I was so pleased to know that our appointment had been scheduled for the week before the week of spring break.
Fast track to the appointment, the geneticist’s assistant comes to the room and Richard and I are ready for the list of questions. If there’s one thing I have learned to do is to always do the E-check in, so we are not sitting there answering all the routine questions during the appointment. She comes in and verifies a few things and asks a few questions before the doctor comes in. Before I go on, I have to explain how hesitant Richard was to go see this doctor, as was I, but only because I knew Richard’s first experience was not a positive one. I tried to reassure him that this was under circumstances and that we need to try to keep an open mind. The geneticist comes in and tells us he very much remembers George from when he was born. He had run some genetic testing for George while he was in the NICU, but because Richard was not keen, we didn’t continue seeing him. The doctor does an extensive full body exam on George and turns to us and said he looks fantastic and there was a pause. Richard and I looked at each other in shock, thinking, “Okay, what’s the catch?” I am sure the doctor was confused as to what was happening, but we rarely heard those words come out of doctor’s mouth.
Of course, we still had loads of questions. What did this mean for George? How could we monitor him and does he need full body scans? Could he have growths later on in life? The doctor explained to us that the genetic report was contradictory, so the next step would be for them to contact the lab to confirm some of the findings. In addition, he said that with this gene they typically see fatty tissue growths or tumors specific areas of the body; however, George is not showing any physical markers. He did not skip over the fact that George does have a large head, but overall he is proportionate. In terms of monitoring him, he told us that there was nothing we could do other than have us followed by a vascular doctor, as well as a dermatologist. This would be a check in to ensure that everything looks good in his veins and arteries, and skin. He ended by telling us that for now we will meet annually for a check in, but ultimately the risk of childhood tumors reduces significantly after the age of 7-8.

In addition to all things related to PIK3CA, I wanted to know why the whole exome did not pick up George’s FBN2 gene. This is the gene that was found during my amniocentesis and the same company ran the panel, so I found it interesting that nothing was mentioned. I wondered if it was because it had been deemed of no important significance. The geneticist’s assistant told me that they would send me a consent form to reach out to the lab, but in that, we mentioned that we have been waiting for these results in order to start trying for a third. The doctor said it is a 50/50 chance that our baby would have this gene. This made my stomach turn and I know it made Richard feel uneasy. I am sure the doctor sensed this and quickly told us that this does not mean there will be complications because they cannot say that the FBN2 gene causes George’s heart condition. It is moments like this where I think Richard and I are so connected because I felt that we both knew we would not push the subject and knew we just had to wait for the lab to give more information. Richard was feeling neutral after the appointment and I was feeling relieved. Relieved because George was found to be healthy and reminded myself that we did our due diligence to get as much information as possible. We did the same before starting to try with Jack and he is healthy. The hardest part of it was over.
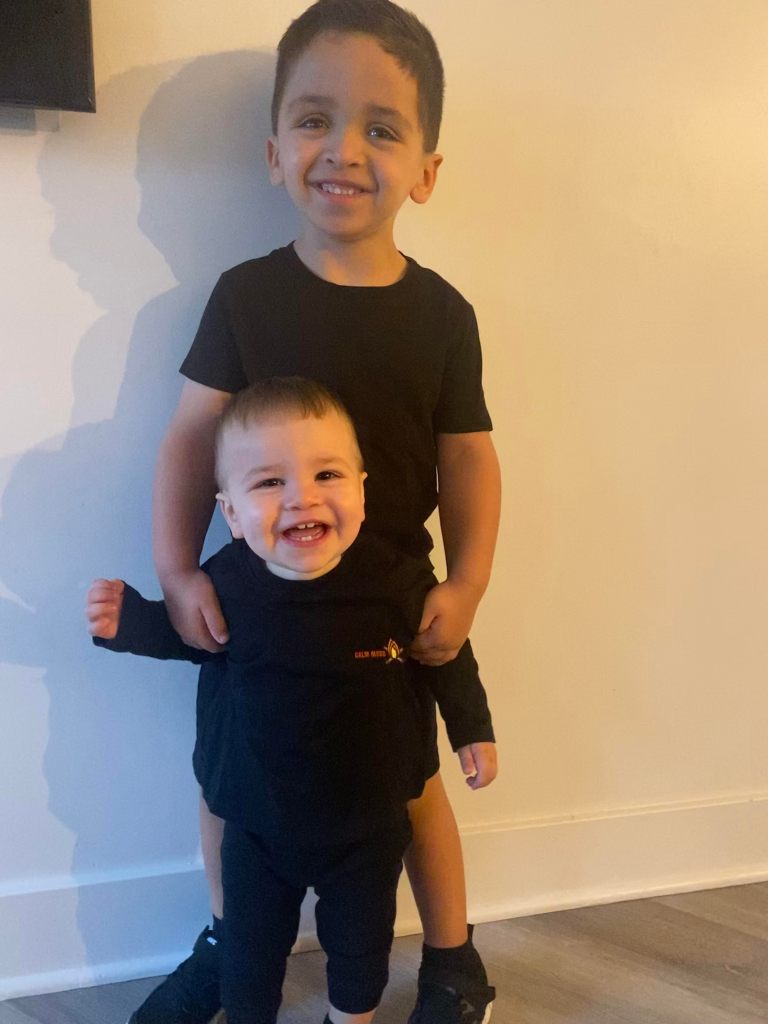
From there, we went to enjoy our spring break in Mexico. George became more comfortable in the water and started jumping in the pool on his own. He is usually a very fearful child, which is the complete opposite of Jack. Jack is entirely fearless, so trying to adjust to both personalities has been a journey. When I say Jack was a blessing to all of us, I mean it. He challenges George and loves him unconditionally. Sometimes I spot Jack really observing George. He watches his every move and when I am having a tough time with him, Jack is patient. He is still and I wonder whether he senses that his brother is different.

In May, we decided with the help of our neurologist that George would start ADHD medication. Richard and I agreed that we would start this the first week of June once we were done traveling for a few weeks. We figured June would be the best time because his teachers knew him very well and they would have June and July to monitor how he does on the medication. The biggest side effects would be trouble sleeping and loss of appetite. The day rolled around and I could not bring myself to give him the medication. I fell into a pit of sadness thinking why my baby. Why does my baby have to take all these pills. So we tried again the next day. George hasn’t had any side effects. A few weeks after starting the medication, George had an EEG scheduled. The following day, my phone rang and I saw the neurologists name pop up. I am sure you see the common theme of my heart sinking. Her secretary said the doctor wanted to relay the message that the seizure medication only seems to be resulting in a slight improvement in George’s brain activity. I told myself that I would not think too much into it and that waiting to see the doctor would be the best thing.
We’re traveling to Seattle Children’s Hospital for a genetics appointment and waiting to see our neurologist next week to plan for next steps.
Having a child on the spectrum is nothing a parent ever plans for or is prepared for. And whether you have a special needs child or not, you have good days and bad days. And so do they. George is gentle and kind, and mischievous and sneaky in his own way. We love him the way he is, but of course as he has grown older, the differences have become much more apparent. He does not like kicking or throwing a ball like any 5-year-old boy would. He talks to himself and repeats many of the things he heard throughout the day over and over again. He finds comfort in the things that made him happy as a baby such as watching specific TV shows (that he has memorized), or singing twinkle twinkle little star. George struggles with social interaction and although children gravitate towards him, it is hard for him to feel connected to other children. He feels much more comfortable around adults. Enter the misconception about autism. People on the spectrum love being on their own. George is a very affectionate child, and loves giving and receiving hugs, from people he knows. At the same time, I know that he tends to get overwhelmed around a group of people and removes himself from the situation. He is not able to tell us that he feels this way, but we try to support him and give him as much space as he needs, while also ensuring he acknowledges who is around him.

I have been hesitant to share this part of George’s story. It has been 13 months since he was diagnosed and I always told myself that I did not want my child labeled or treated a certain way for being different. As hard as it is sharing, I am taking charge of our narrative. I know that Richard and I will always be George’s best advocates.

I have never felt ashamed of his diagnosis, but in all honesty, I have been fearful of what others would think. Sometimes people see others that they do not know and they are acting differently. I have heard, “Oh, they must be on drugs,” or “he definitely has something.” I do worry about George’s future and I am sure that parents with neurotypical children can also relate because as a parent it is our duty to worry. I guess I worry about other things, like whether he will ever find love, or go to college. I worry about whether George will ever be able to express to me how he is feeling. I worry about him being viewed or treated differently because of his autism. Today, George has wonderful friends, and their parents are incredible. The community we have around us is supportive and resourceful. George has neurotypical friends that adore him and friends with ASD that adore him, but as children grow older the innocence starts to fade. I encourage everyone to educate themselves and educate their children and loved ones- to just be kind.